For many people turkey is a beloved staple that graces holiday tables and provides a lean, protein-packed option for sandwiches and meals year-round. But for some turkey isn’t just another dietary choice – it’s an allergen. Turkey meat allergy, while less common than other food allergies, is quite real and can cause concerning reactions in sensitive individuals.
Understanding the symptoms, testing procedures, and management strategies for turkey meat allergy empowers affected individuals to make informed choices and safeguard their health. Here is a comprehensive guide to what you need to know about turkey meat allergy
What are the Symptoms of Turkey Meat Allergy?
Reactions to turkey meat can vary widely, from mild to severe:
-
Oral Allergy Syndrome: Itching, tingling, or swelling of the lips, tongue, mouth and throat after eating turkey.
-
Gastrointestinal Distress: Nausea, vomiting, diarrhea, abdominal cramping after turkey ingestion.
-
Skin Reactions: Hives (raised, itchy welts), eczema flares, or swelling around the face, lips and eyes.
-
Anaphylaxis: A potentially life-threatening reaction involving impaired breathing, throat swelling, low blood pressure, dizziness and fainting. Requires immediate medical treatment.
-
Rhinitis: Stuffy, runny nose and sneezing after exposure to cooking turkey odors or steam.
Reactions usually start within minutes to a few hours after eating turkey. The severity can range from mild discomfort to anaphylaxis.
What Causes Turkey Meat Allergy?
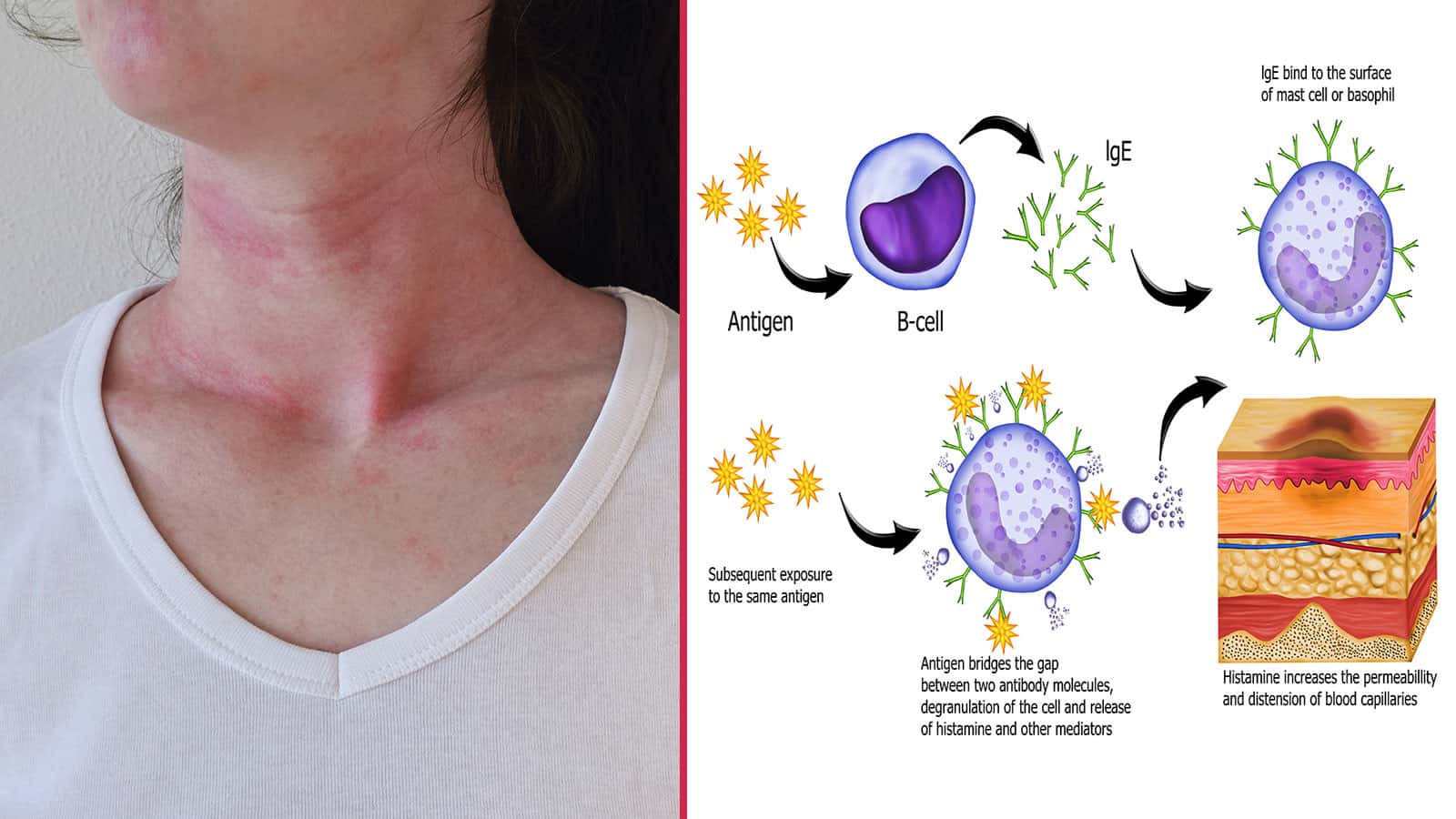
Turkey meat allergy is prompted by the immune system mistakenly identifying turkey proteins as harmful. This spurs the release of IgE antibodies that trigger the above allergic reactions upon re-exposure.
Several potential causes exist:
-
Cross-reactivity: Allergy to other poultry like chicken or duck, or eggs, as these all contain similar allergy-provoking proteins. Up to 35% of children with egg allergy react to turkey.
-
Tick bites: The Lone Star tick can spark new meat allergies, including turkey, through substances in its saliva. Most common in the Southeastern U.S.
-
Genetic predisposition: Family history of allergies increases risk.
How is Turkey Meat Allergy Diagnosed?
Allergy testing helps confirm turkey as the trigger:
-
Skin prick test: Drops containing turkey protein extracts are placed on the skin. A positive result is itching and redness at the test site.
-
Blood test: Measures levels of turkey-specific IgE antibodies in the blood. Higher levels indicate an allergy.
-
Elimination diet: Removing turkey from the diet, monitoring symptoms, and later reintroducing it can help identify reactivity.
-
Oral food challenge: Gradually feeding increasing doses of turkey under medical supervision to definitely confirm or rule out an allergy.
What is the Treatment for Turkey Meat Allergy?
Strict avoidance of turkey meat and products containing turkey derivatives like broth or gelatin is the mainstay of treatment. Thoroughly checking ingredient labels is crucial.
Other management precautions include:
- Carrying epinephrine (Epipen) if anaphylaxis is a concern
- Avoiding use of turkey-derived cosmetics, pet foods, etc.
- Washing hands and surfaces after handling turkey to prevent contact reactions
- Letting friends and family know about the allergy
- Working with a registered dietitian to identify substitute protein sources
For milder allergies, some people may tolerate limited turkey exposure or fully cooked products. Discuss options with an allergist.
Turkey Allergy vs. Turkey Sensitivity
Some people experience gastrointestinal distress or other symptoms after eating turkey but lack an allergy. This represents a non-allergic sensitivity or intolerance. Allergies involve the immune system, while sensitivities do not.
Can You Outgrow a Turkey Allergy?
For children who develop a turkey allergy, it is possible to outgrow it over time. But allergy persistence into adulthood is also common. Periodic follow-up testing can help identify if the body’s reactivity has resolved.
Key Takeaways on Turkey Meat Allergy
While less prevalent than many other food allergies, turkey allergy is quite possible and can range from mild to severe. Diagnosis via medical testing provides definitive confirmation so proper avoidance and treatment steps can be followed.
Understanding symptoms, management tips, and when to seek emergency care allows those with turkey allergy to stay safe and healthy. Being well-informed is key to thriving with this condition.
Frequency of Entities
- turkey: 27
- allergy: 24
- meat: 16
- symptoms: 7
- gastrointestinal: 5
- anaphylaxis: 5
- testing: 4
- treatment: 3
- intolerance: 2
- sensitivity: 2
- proteins: 2
- ingestion: 2
- avoidance: 2
Managing a severe food reaction with epinephrine
Food allergies, like meat allergies, can have symptoms that are mild to life-threatening. It’s hard to say how bad each reaction will be. People who have previously experienced only mild symptoms may suddenly experience a more severe reaction, including anaphylaxis. In the US, food allergy is the leading cause of anaphylaxis outside the hospital setting.
Epinephrine is the first medicine that is used to treat anaphylaxis, which happens when an allergen makes your body release a lot of chemicals that could put your body into shock if you don’t treat it right away. Anaphylaxis can occur within seconds or minutes, can worsen quickly, and can be deadly.
If you have a food allergy, your allergist will probably give you an epinephrine auto-injector and show you how to use it. Check your auto-injector’s expiration date, write it down on your calendar, and ask your pharmacy if they offer services that will remind you when it’s time to renew your prescriptions.
If you can, have two epinephrine auto-injectors on hand, especially if you will be far from emergency care, because the severe reaction could happen again. Epinephrine should be taken right away if you have severe symptoms like shortness of breath, coughing that won’t go away, hives all over your body, a sore throat, trouble breathing or swallowing, or a mix of symptoms from different parts of your body, like hives, rashes, or skin swelling along with vomiting, diarrhea, or abdominal pain.
If you’re not sure if a reaction needs epinephrine, you should still give it because the benefits are greater than the risks.
Common side effects of epinephrine may include anxiety, restlessness, dizziness, and shakiness. If you have certain pre-existing conditions, you may be at a higher risk for adverse effects with epinephrine.
Your allergist will give you a written emergency treatment plan that tells you what medicines to give and when.
Once epinephrine has been administered, immediately call 911 and inform the dispatcher that epinephrine was given.
Antihistamines and albuterol are two other medicines that may be given to treat food allergy symptoms. However, it is important to remember that epinephrine is the only medicine that can reverse the life-threatening symptoms of anaphylaxis. These other medicines can be given after epinephrine, and your food allergy action plan may say that antihistamines alone can be given for milder allergic reactions.
How to tell if you have a food allergy, according to a nutritionist
FAQ
What are the symptoms of turkey allergy?
Can you be allergic to turkey but not chicken?
What meat are people most allergic to?
How do you know if you have a meat intolerance?
Do you have a meat allergy?
A meat allergy can develop any time in life. If you are allergic to one type of meat, it is possible you also are allergic to other meats, as well as to poultry such as chicken, turkey and duck. Studies have found that a very small percentage of children with milk allergy are also allergic to beef.
Why is meat unhealthy for you?
Meat is actually healthy. What can sometimes make its daily consumption inadvisable are those meats or cuts that have a high percentage of fat. However, they are a great source of proteins of high biological value, iron and B complex vitamins.
Is there a link between meat allergies and other foods?
Researchers have found a number of links between meat allergies and other foods too, especially with a primary beef allergy (not caused by alpha-gal). Beef allergy in children who have a cow’s milk allergy may be found in up to 20% of cases. Other foods to avoid include:
Is Turkey lethargy a symptom of an allergy?
Many attribute this lethargy to the turkey eaten on Thanksgiving. Many feel that they are having an allergic reaction to turkey due to this somnolence, however, it is not an allergy at all. Allergies to turkey meat are not common, but a true allergy to turkey can occur in some individuals.
Can a meat allergy be caused by a mammal?
Meat from any kind of mammal — beef, lamb, pork, goat, and even whale and seal — can cause an allergic reaction. While meat allergy is uncommon, more cases have been reported in the past few years and the numbers continue to rise due to increased recognition of the diagnosis.
Do you have a red meat allergy?
This allergy is known as alpha-gal syndrome, commonly called red meat allergy. It can affect people who eat beef, pork, bison, lamb, venison and/or goat. How does this happen? You get bitten by a tick (usually the lone star tick) and that bite transfers alpha gal, a type of sugar molecule found in your body.